By Abigail Schanfield, Benjamin Brooks
Over the last decade, buzzwords like “health equity” and “social determinants of health” have dominated the attention of both academic and medical experts. In a New England Journal of Medicine Perspective titled “Ensuring That LGBTQI+ People Count – Collecting Data on Sexual Orientation, Gender Identity, and Intersex Status” researchers and community advocates Kellan Baker, Carl Streed Jr, and Laura Durso remind medical providers we can help mitigate the significant health disparities experienced by LGBTQI+ patients through routine data collection.
Inquiring about social determinants of health (SDOH) like housing, employment, and income help providers support patients’ overall health, improve collaboration on treatment plans, and help providers understand which patients might be in danger of slipping through the cracks of our social safety net.
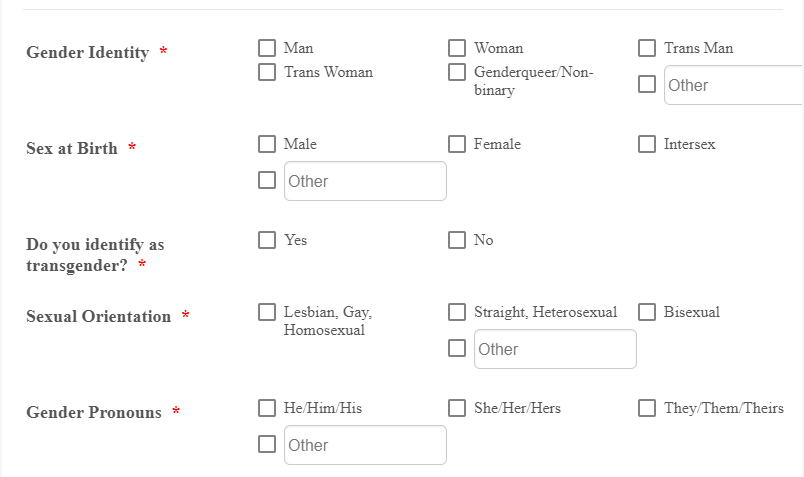
Sexual orientation and gender identity (SOGI) data collection offers a similar promise. However, less attention has been given to why asking patients about their SOGI data is so critical to ensuring quality care. SOGI data help providers meet clients where they’re at and push us to see beyond clinical diagnoses to the whole person, helping us consider all the pieces of the human experience. At Whitman-Walker, our motto is “We See You.” Our tagline encapsulates the important role SOGI data can play in ending the inequities experienced by LGBTQI+ patients.
In our patient-centered care model, from the moment a patient walks in the door they are welcomed by our client services staff with the name they go by and their pronouns. This sense of affirmation is part of why we can openly discuss sensitive health topics with our patients. Affirmation leads to honesty. A patient and their provider can more openly discuss topics like pathways to hormone replacement therapy, harm-reduction for drug use, or life challenges outside the clinic if patients feel safe and seen by their provider.
When our patients can be truly seen for who they are, we can make appropriate referrals for housing services, or our legal team can support a patient navigate the convoluted process of changing their name or gender marker on their government documents. Through the process of SOGI data collection, we can celebrate with our clients through their many affirming milestones and create space for grief when an LGBTQI+ patient or the larger community experiences loss or violence.
In addition to building rapport with our patients, SOGI and SDOH data help us understand and combat drivers of disparities across all aspects of our patients’ lives. As providers, we cannot fully understand the intersections of gender identity or sexual orientation and substance misuse, chronic illness, incarceration, employment status, or how LGBTQI+ people are faring through COVID-19 if we do not have the data. As medical providers, data collection is how we innovate and evolve as a profession. Data is the key to fulfilling the promise of medicine to benefit society as a whole.
It is still common for many doctors and medical personnel to express reticence about asking patients for their SOGI status. We have been conditioned to believe sex, gender, and sexual orientation are strictly personal and are not relevant beyond our patients’ private lives. At Whitman-Walker, by contrast, we grapple with the complexities of gender and sexuality every day, and we watch our patients benefit because of it. Recognizing the important role SOGI data play in health care, the National Institutes of Health have recently commissioned the National Academies of Sciences, Engineering, and Medicine to develop a report with recommendations on how best to collect data on sex, gender, and sexual orientation.
Meaningful engagement paired with data collection opens doors for medical providers to be more innovative and creative when supporting not only our LGBTQI+ patients, but our entire patient population. As providers, we have an obligation to provide quality care to all our patients. SOGI data is embedded in a larger story. Engaging with our patients to truly understand those stories about their lives can help us create meaningful programs to improve our patients’ health and engagement in care, adjust our administrative systems to better serve our patients, and build a health care system that works better for everyone.


